The evaluation of essential elements defining varicose vein mapping
Claude Franceschi, Stefano Ermini
Preliminary notes
- DUS check-up must be done with the patient standing and with the feet resting on the floor. This allows the re-creation of a physiologic movement during dynamic flow activation tests with the patient standing in front of the physician.
- The detected flow must be put in relation to the kind of activation flow test used, and to its phase (muscle pump contraction/relaxation, Valsalva press or release, systole/diastole).
Great saphenous vein
Anatomic US check-up
- Record the presence/competence/incompetence of the anterior accessory saphenous vein (pay attention to the alignment sign).
- Record SFJ anatomical aberrations (double SFJ, superficial femoral artery position, dilations and tributary disposition if in a prominent position).
- Measure the GSV trunk caliber 15 cm below the groin with exclusion of the dilations.
- Record the number of dilations.
Hemodynamic check-up
- Record competence/incompetence of the saphenous trunk.
- Record the presence of an escape point, specifying the test used.
- Record the presence of one or more pelvic escape point as described by C. Franceschi.
- In case of SFJ incompetence, specify the competence/incompetence of the terminal valve, with reference to the tests used and evidencing the incongruences.
- Define GSV length incompetence and any multiple incompetence segments.
Small saphenous vein
Anatomic US check-up
- Record the SPJ height level.
- Record the relationship with the gastrocnemius veins.
- Record the presence or not of the Giacomini Vein and of the thigh extension vein.
- Measure the SSV trunk caliber below the junction.
Hemodynamic check-up
- Use only the PARANA’ maneuver.
- Record the competence/incompetence of the SPJ terminal valve.
- Record the SSV length incompetence and any multiple incompetence segments.
- Look for the presence of a systolic reflux and define its duration in relation to the muscle pump contraction phase.
- Look for the flow direction in the convexity or concavity arc tributaries.
- In case of simultaneous Popliteal vein incompetence, repeat the check-up associating the SSV trunk finger compression below the junction.
Perforators (anatomically enlarged)
- Use only dynamic tests (Paranà, knee bending).
- Record its role in relation to its hemodynamic pattern, keeping in mind that:
- Diastolic inward flow is typical of a re-entry perforator.
- Diastolic outward flow is typical of an escape point Stefano Ermini & Claude Franceschi.
- Systolic outward flow is typical of vicarious (compensative) flow in a shrinking syndrome and is always facilitated by its angle of insertion.
- A systole refluxing perforator can also represent the escape point of a varicose vein, in absence of deep vein dysfunction. This is due to the perforator angle and is always the consequence of a trauma. In this perforator the diastolic behavior is conditioned by the fact that the gradient level may or may not generate a syphon effect (height of the hydrostatic column interposed between the escape point and the re-entry perforator and possible diastolic muscular choking) and by the competence of the higher venous system.
- AsSysto-diastolic outward flow is the typical pattern of an incompetent perforator associated with the absence of orthodynamic pressure fractioning in the deep veins.
- The absence of flow is due to the absence of gradient and this may be related to the type of valve competence test used, to a simultaneous and deep vein incompetence, or to the fact that the patient has been standing for a long time. g. A GSV perforator placed in a non-terminal area may present a diastolic outward flow that must not be considered pathogenic (please measure the GSV caliber above and below the perforator). This diastolic outward flow inverts its direction closing the GSV below the perforator (finger compression or surgical disconnection).
Giacomini vein
Check the flow direction using a Paranà maneuver
- If the flow is centrifugal (towards the SPJ):
- Find an escape point (if one exists)
- Determine if the centrifugal flow is Valsalva positive or negative.
- If the flow is centripetal (distancing from the SPJ):
- Check if the systolic shunt is an open derivative or vicarious (if it is sustained or not by a compensative function)
- Check the centripetal flow duration in relation the muscle pump contraction phase (if it occurs only in the early contraction or if it is present during the entire muscle pump contraction phase)
- Compare the right and left calibers of the femoral superficial vein
- Repeat the test with a shoe that has a 4 cm heel
- Points b, c, and d can be considered part of a pre-surgical exam and not a first level Doppler US check up.
Reccomendations
- Superficial veins: it is absolutely useless to measure the reflux time in order to relate it to the presumed gravity of the SVI, because reflux time depends on the gradient exhaustion time. This time depends on the kind of valve competence test used and on the filling level of the venous system at the time the test is performed.
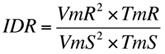
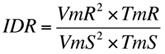
- Deep Veins: Dynamic Reflux Index proposed by C. Franceschi can be used
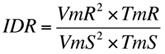
(VmR=average diastolic reflux speed, TmR=average diastolic reflux time, VmS= average systolic speed, TmS= average systolic time)
- It is mandatory to identify without hesitation the vicarious circles (compensative circles). Their disconnection leads to a huge worsening that is no longer curable (if not by nature).
- Remember that our mission is to cure the patient and not to treat the reflux.
- Use the Perthes test to clarify ambiguous situations during DUS check-up and to limit unnecessary and extensive phlebectomies in the surgical planning phase.
Basic venous mapping elements useless to plan a hemodynamic conservative strategy (to add to what is described above)
The mission of Hemodynamic Conservative Surgery is to preserve a draining saphenous system.
The saphenous drainage after hemodynamic correction can be restored with a centrifugal flow or with a centripetal flow.
- Basic elements to restore a centrifugal non-pathogenic saphenous flow:
- To convert a closed diastolic shunt in a open diastolic derivative shunt (to treat the escape point N1-‐>N2, N2-‐>N3).
- To restore a physiologic compartment drainage (from N3 to N1).
- The finger tributary compression test can be used in the definition of re-entry perforators.
- In case of GSV trunk disconnection below a perforator (<1%), check the saphenous flow with a dynamic test compressing the GSV trunk below the perforator.
- Basic elements to restore a centripetal non-pathogenic saphenous flow:
- To test centripetal saphenous flow speed and time after finger tributary compression using a dynamic maneuver. This is important when we choose the strategy treatment of a type IIb shunt.
- To test the relation between the incompetent GSV caliber and that of the competent tract as well as the length of both segments.
- To check GSV trunk multiple incompetences.
More information in:
https://drive.google.com/file/d/0B9u_dUXdRAPYbUZqUzRvelBQZXc/view?usp=sharing
http://www.slideshare.net/ClaudeFranceschi/duplex-assessment-of-venous-hemodynamics-3-oct-13th-2011-‐morning-20mn2
[TOP]