
a Office of the WHO Representative in the Philippines, Sta Cruz, Manila, Philippines.
b Regional Office for Eastern Visayas, Department of Health, Tacloban City, Philippines.
c Department of Health, Sta Cruz, Manila, Philippines.
d Division of Communicable Diseases, World Health Organization Regional Office for the Western Pacific, Manila, Philippines.
e National Centre for Epidemiology and Public Health, Australia National University, Canberra, Australia.
Correspondence to Lasse S Vestergaard (email: lasse.vestergaardl@dadlnet.dk).
To cite this article:
Aumentado C et al. The prevention and control of dengue after Typhoon Haiyan. Western Pacific Surveillance and Response Journal, 2015, 6(Suppl 1):60–65. doi:10.5365/wpsar.2015.6.3.HYN_018
Objective: Many of the areas in the Philippines affected by Typhoon Haiyan are endemic for dengue; therefore, dengue prevention was a priority in the initial post-disaster risk assessment. We describe the dengue prevention and response strategies applied after Haiyan.
Methods: The dengue response was implemented by a wide range of national and international stakeholders. Priorities included the rapid re-establishment of an effective surveillance system to quickly identify new dengue cases, monitor trends and determine the geographical distribution of cases. Dengue rapid diagnostic tests (RDTs) were distributed to sentinel health facilities, and comprehensive vector control activities and entomological surveys were implemented. Several training sessions for key stakeholders and awareness campaigns for communities were organized.
Results: There were RDT-positive dengue cases reported from urban and semi-urban areas where entomological surveys also confirmed a high density of Aedes aegypti mosquitoes. Although there was an increase in dengue cases in January 2014, the number of cases remained below the epidemic threshold throughout the remaining months of 2014.
Discussion: There was no large outbreak of dengue after Typhoon Haiyan, possibly due to the targeted, multifaceted and rapid response for dengue after Haiyan. However, surveillance differed after Haiyan, making comparisons with previous years difficult. Multiple players contributed to the response that was also facilitated by close communication and coordination within the Health Cluster.
Dengue is endemic in the Philippines, with the number of notified cases ranging from less than 20 000 in 20051 to 204 906 in 20132 and 113 485 in 2014.3 Although these case numbers reported from health facilities through the national surveillance systems are high, the actual case burden has been estimated to be seven times higher.4 Dengue epidemics occur at three- to four-year intervals, with the most recent epidemic experienced in 2010.1 Fortunately, while the notification rate of dengue cases has increased in the Philippines in recent years, the case fatality rate has declined1 following the introduction of new national clinical dengue case management guidelines. These are based on the latest global guidelines issued by the World Health Organization (WHO)5 and have been implemented through comprehensive training of doctors and nurses nationwide. While dengue transmission occurs year-round, a sharp increase is usually observed between July and October, the main rainy season, when there is increased mosquito breeding. There is also a smaller peak observed around January.6 Dengue prevention efforts and public health campaigns are permanently implemented at various levels by national, regional and provincial health authorities, but are intensified before these dengue peak seasons, particularly in established high-risk areas.
Dengue outbreaks are common after natural disasters such as earthquakes, typhoons and floods.7 Typhoon Haiyan, which hit the Philippines on 8 November 2013, rapidly destroyed or damaged houses, health facilities and infrastructure on a devastating scale.8 Sustained rainfall in subsequent weeks resulted in the excessive accumulation of debris with stagnant water. Both provided the potential for a large increase in mosquito breeding sites, leading to an expanding mosquito population and a higher risk of dengue transmission. The dengue-endemic areas of Region 8, with its six provinces and a population of around 4 million people,9 was severely affected by the typhoon.
Given the potential for a large dengue outbreak following Haiyan, the WHO public health risk assessment for Typhoon Haiyan recognized dengue fever as one of the health priorities for the affected areas with a potential increase in cases occurring in the six weeks post-typhoon.10 The aim of the response to dengue was to prevent an outbreak in the immediate aftermath of the typhoon and to reinstate dengue control, surveillance and response capacity ahead of the usual peak season that would follow in the year after the typhoon. This paper describes the dengue prevention and response strategies applied after Haiyan in Region 8.
Notifiable diseases are reported weekly to the Philippine Integrated Disease Surveillance and Response System (PIDSR);11 frequency was increased to daily reporting for dengue and seven other priority diseases 10 days after Haiyan from eight hospitals/mobile clinics within and near Tacloban City. The standard case definitions for dengue cases with warning signs and probable dengue cases were used.6 However, post-Haiyan probable dengue cases also included those cases who had a positive rapid antigen-antibody test.
Additional health personnel from the Department of Health (DOH), foreign medical teams and response consultants worked in surveillance reporting and case investigations. Alerts for dengue – clustering of cases or a death of a suspect dengue case – were also reported through event-based surveillance (ESR). In the Philippines, an outbreak is considered when the number of reported dengue cases exceeds the epidemic threshold, i.e. the average number of cases reported in the previous five years.
Surveillance in Post Extreme Emergencies and Disaster (SPEED)12 was also activated three weeks after Haiyan at selected sites such as evacuation centres and rural health units. Reports of acute haemorrhagic fever (AHF) cases were monitored as these can be dengue cases, with any cases or deaths reported immediately referred to the Regional Surveillance and Epidemiology Unit (RESU) for further verification and investigation. SPEED runners with motorbikes were hired to facilitate data collection and submission to the provincial level for analysis to be reported to the regional and national level.
Updated maps of dengue cases were produced by the RESU and shared among dengue programme coordinators and with health partners at Health Cluster meetings.
Four weeks after the typhoon, commercial antigen-antibody combination dengue rapid diagnostic tests (RDTs) were strategically distributed to eight selected hospitals/health centres in Region 8. The purpose was to determine the proportion of RDT-positive dengue cases (i.e. probable dengue cases) among all reported suspected cases and to establish the presence of dengue in an area. Primarily index cases were tested, and RDT-positive cases were reported to RESU for mapping to guide rapid response measures and targeted interventions. RDT results were not confirmed by serology and virus isolation.
Treatment of cases followed the standard clinical criteria. Clinical guidelines on dengue case management were provided to hospitals and health centres together with refresher training of health staff from all typhoon-affected areas by DOH, local health authorities and international partners.
Vector control operations, which involved fogging (space spraying), larvaciding (primarily applying the chemical pyriproxifen) and search-and-destroy activities were initiated 12 days after Haiyan. Areas located around hospitals, damaged schools, evacuation centres and other public places were systematically targeted. Later, when case-based surveillance had been re-established, vector control operations were conducted based on reported dengue cases. As the local vector control capacity was disrupted, vector control activities were supported by staff from other regions and by foreign medical teams and military. Additional fogging equipment and insecticides were provided, following national standard requirements and specifications.
A series of entomological assessments were conducted by WHO and regional health authorities in Tacloban City, Ormoc City and in some selected municipalities three months after the typhoon to identify the main dengue vector breeding sites, assess the vector density after the typhoon and evaluate the effect of vector control interventions. The Breteaux index was determined in each locality following standard procedures.13 Sanitation inspectors and community-based village dengue brigades were trained on vector surveillance and integrated vector control. DOH also promoted search-and-destroy activities with the support of the village dengue brigades. Entomological data collection was repeated following vector control cycles to monitor reductions in mosquito numbers.
There were 164 dengue cases with warning signs reported in Region 8 through PIDSR between 8 November and 31 December 2013. For 2014, there were 5227 dengue cases reported with 20 deaths (case fatality rate [CFR] = 0.4%), a 61% increase in cases compared to 2013 (n = 3254). Ages of cases ranged from 29 days to 88 years (median: 13 years old). The number of cases exceeded the epidemic threshold in January 2014 but not again during 2014 (Figure 1).

* Epidemic threshold is the average annual number of cases reported in the previous five years.
PIDSR, Philippine Integrated Disease Surveillance and Response.
Among the 5227 dengue cases in 2014, 1490 (29%) were tested with RDTs and 1172 were positive (79%). There was a clustering of RDT-positive cases in urban and semi-urban settings (Figure 2) where the most debris accumulated due to the typhoon.

There were 31 cases of AHF reported through SPEED from Leyte province who were hospitalized between 11 and 25 November 2013. Four cases of suspected dengue were reported through ESR in Leyte province from 1 to 7 December 2013.
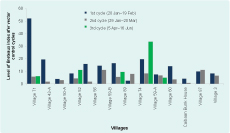
There were two to three cycles of integrated vector control operations and vector surveillance data collection administered at one- to two-week intervals in the 14 targeted villages in Tacloban City. Local health offices had limited capacity for vector control due to reduced human resources and logistical support. Community participation in assessing household activities to eliminate breeding sites was low.
Entomological surveys were undertaken three months post-Haiyan and comprised at least 100 households in each locality, except one locality where only 85 households were included (average: 302; median: 159; range: 85–973). Overall, the surveys found a high density of Aedes aegypti mosquitoes in all surveyed institutions and areas. In Ormoc City, only Aedes aegypti was detected, while in Tacloban City, both Aedes aegypti and Aedes albopictus were detected. The Breteaux index decreased between the first and second cycles in many villages (Figure 3) as did the House index and Pupal index (data not shown). The Breteaux index decrease was most marked in Village 71 of Tacloban City where after a three-week interval it decreased from 52 to 6; the House index also decreased from 20% to 5%, as did the Pupal index from 233% to 56% over three vector control cycles.
The most common containers with mosquito breeding observed were discarded containers (50%), tyres (18%), home utensils (11%), water storage tanks (6%), flower pots (5%), rainwater harvesting drums (3%), removed roof covers (3%) and others (4%).
WHO and DOH conducted workshops on dengue clinical case management, vector surveillance, vector control, social mobilization and the case surveillance system. There were 128 health staff from different provinces and municipalities trained on clinical case management and a total of 199 participants in trainings overall (from 14 hospitals, eight local health units and 71 villages).
A series of advocacy activities were conducted by DOH and partner organizations: distribution of information, communication and education materials; broadcasting of radio messages and radio guest speakers; and other health promotion activities. Awareness was also heightened among foreign aid workers following a small cluster of dengue cases among them.9 Long-lasting insecticide-treated nets were distributed to selected government hospitals to prevent transmission to patients and staff.
A multifaceted response was rapidly initiated for the prevalence and control of dengue post-Haiyan from many stakeholders, including national and regional health authorities and local and international agencies. Although the number of dengue cases reported in Region 8 in 2014 was higher than in 2013, there were no outbreaks reported and the epidemic threshold was only exceeded in January 2014. This observed increase may partly be due to the initial efforts for dengue surveillance, increased attention and awareness and the use of RDTs at sentinel health facilities. As RDT-positive cases were included in the probable case definition after Haiyan, caution is required when making comparisons with previous years.
Reducing dengue transmission was one of the initial priorities of the response to Haiyan,10 and this was achieved through strengthening dengue surveillance for early detection and through targeted vector control. Moving to daily reporting of dengue cases through PIDSR and SPEED allowed for earlier identification of cases with the directed targeted vector control efforts. This timeliness limited the potential spread. Using maps of cases also assisted in targeting vector control in real time.
The use of RDTs also contributed to early diagnosis and targeted vector control as they increased the specificity of diagnosis. In non-emergency times, an increase of clinically suspicious dengue cases usually occurs during the peak season from July to October so that cases presenting with flu-like symptoms are diagnosed with dengue without any laboratory confirmation. Ideally, RDT-positive cases should have been confirmed with further laboratory tests, at least for a subset of samples, but this was not feasible given the circumstances. Despite this, the use of RDTs in selected health facilities helped improve the diagnostic accuracy of dengue and allowed for suspected outbreaks of dengue to be confirmed as not being dengue, especially in the early response.
The early vector control activities that occurred post-Haiyan comprised of space spraying and chemical larviciding, and these were initially conducted sporadically across affected areas without any entomological evidence base. Although wide-scale spraying is not advocated for the prevention of dengue except in outbreak situations,13 this initial spraying did appear effective in reducing mosquito densities particularly in evacuation centres and hospitals. However, further evidence is required to determine the efficacy of such control strategies.14 Larviciding of mosquito breeding sites and around debris and garbage collection areas also reduced mosquito and fly densities, which was important due to the continuous rainfall in the months following Haiyan that increased mosquito breeding sites. The continued rain also encouraged more indoor time that can lead to increased exposure to indoor Aedes aegypti species.
There are several limitations in this assessment, most of which relate to it being conducted in a post-disaster situation. There was not sufficient entomological data to draw firm conclusions about the effect of vector control interventions, and the exact size of the population denominator in specific geographical locations was unknown. Therefore it was difficult to determine the extent to which the emergency response reduced and prevented transmission of dengue. Changes to the case definition also prevents detailed comparisons with previous years. However, based on the limited data available, and the fact that the epidemic threshold was only exceeded in January 2014, it appears that the response to dengue was effective. This was achieved despite many operational challenges and adverse conditions for the dengue prevention efforts. Close collaboration among the local community, DOH, WHO and numerous national and international organizations ensured that dengue cases were detected early and targeted responses were quickly implemented, thus successfully minimizing widespread cases of dengue in Region 8. The lessons learnt and the increased local capacity built in Region 8 as part of the response to dengue after Typhoon Haiyan will likely benefit both in emergency and non-emergency responses in the future.
None declared.
None.
The authors sincerely acknowledge the contributions of every individual and institution involved in the response to dengue and all other health problems caused by Typhoon Haiyan in the Philippines.